As outlined by the Centers for Medicare and Medicaid Services (CMS), Complying with Medical Record Documentation Requirements remains critical to senior care success.
Proper documentation:
- Helps patients get reasonable and necessary items/services
- Facilitates proper claim payment
- Supports favorable medical review decisions
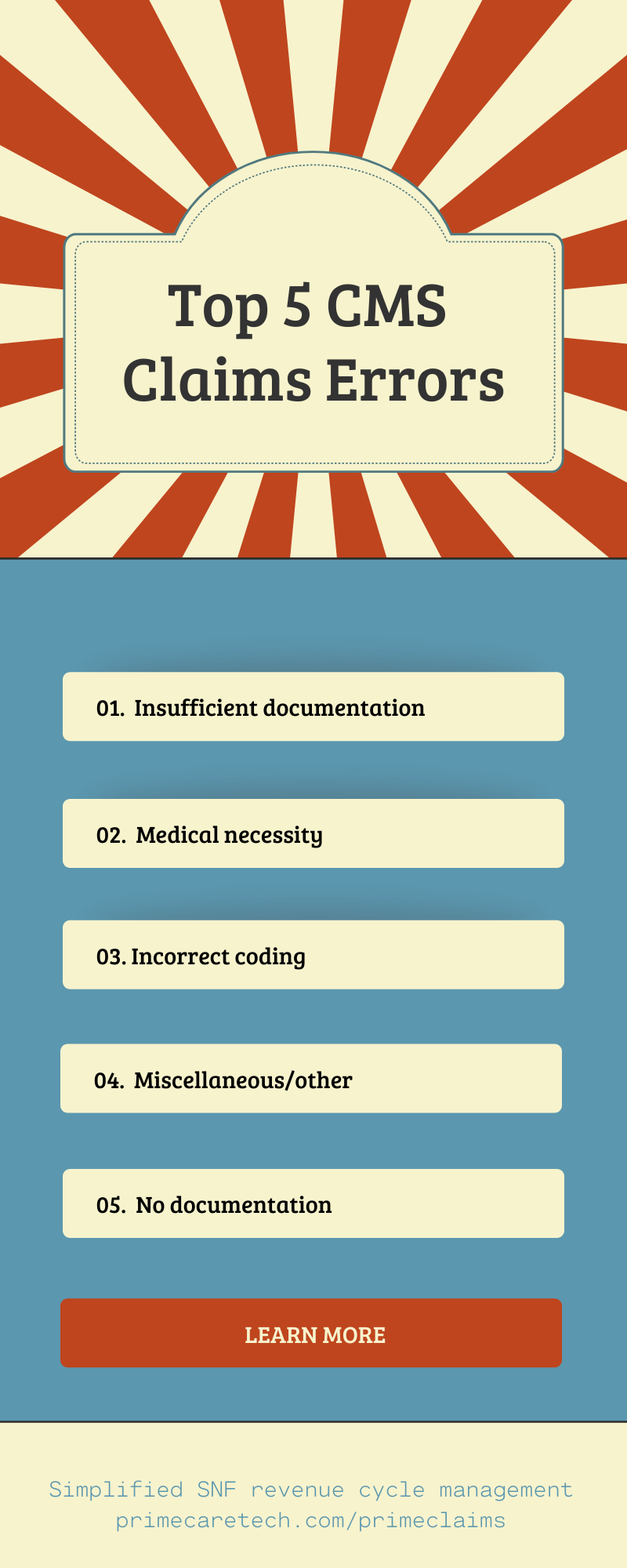
Specific to claims reimbursement, CMS identified the top five reasons for errors. Note, two are related to documentation.
So, what does insufficient documentation mean?
- It does NOT mean documentation doesn’t exist.
- It means something was incomplete or missing at claim submission.
And, what are the consequences of improper documentation?
Improper documentation disrupts the revenue cycle, which results in loss of financial revenue. CMS claim denials also cost your staff time, requiring them to:
- Complete forms
- Submit additional documentation
- Send a letter explaining why the claim should be paid
- Resubmit claim
Secondarily, if your order for item/service is illegible, your patient care suffers.
What are some tips for improved documentation?
- Send ALL associated documentation supporting the item/service billed
- Some information may come from a prior claim or test
- If you're not sure if certain documentation is required, send it anyway
- Send the documentation by the deadline indicated in the request
- Review documentation to make sure it:
- Answers who, what, when, why, and how
- Verifies item/service was performed
- Verifies medical necessity
Where can I get more information regarding CMS claims errors, including documentation?
- Complying with Medical Record Documentation Requirements
- Complying with Medicare Signature Requirements
Lastly, senior care and skilled nursing facilities (SNFs) can greatly simplify claims revenue management by employing a system customized for this industry, and supported by seasoned claims professionals. Get in touch if we can help.
/Prime-Care-Technologies-Logo.png?width=191&height=55&name=Prime-Care-Technologies-Logo.png)