The Federal Communications Commission (FCC) and Centers for Medicare & Medicaid Services (CMS) are making it more lucrative than ever for senior care facilities to toe-test telehealth – and they’re no longer catering to just rural facilities.
FCC Funding
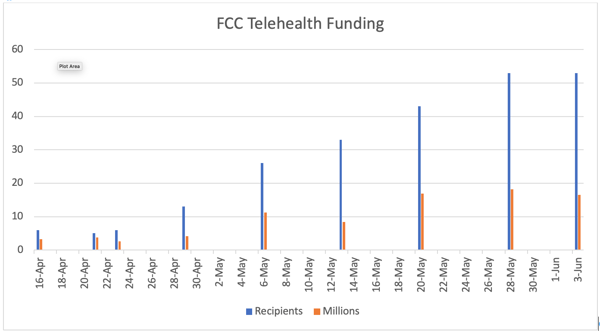
To date, the FCC’s COVID-19 Telehealth Program has approved funding for 238 health care providers:
- Urban and rural
- In 41 states plus Washington, D.C.
- Totaling $84.96 million (of $200 million available)
This means there’s 58 percent – $115 million – in funding still on the table.
Criteria to award funding
- Conditions to be treated
- Goals and objectives for use
- Timeline for service/device deployment
- Factors/metrics used to measure impact
- Geographic area/ population served (pre-existing strain, provider shortages, rural closures, limited broadband and/or internet adoption)
- Ability to target high-risk and vulnerable patients
Resources
- FCC COVID-19 Telehealth Program
- FCC COVID-19 Telehealth Program FAQs
- FCC COVID-19 Telehealth Program Recipients
CMS Changes
Meanwhile, effective March 6 and for the duration of the COVID-19 emergency, Medicare is willing to pay clinicians the same fee for services rendered via telehealth to any beneficiary anywhere (e.g., treat-in-place). Previously it was limited to rural SNFs and/or required patients to come to a telehealth facility for treatment. Now various clinicians, including specialists, can treat your patients right in your facility and all skilled nursing facilities are eligible.
And, don't be put off by the 'temporary' implication of this change. Word has it, CMS may make temporary telehealth provisions permanent, based on positive results.
Resources
- CMS List of Telehealth Services
- CMS Medicare Telemedicine Provider Fact Sheet
- Verma favors keeping expanded telemedicine access after pandemic
Conclusion
With telemedicine trending as it is, make sure you take time to understand the funding available and get a slice of that pie. What's more, this may be the fix you've been looking for to fill staffing gaps. Virtual treatment grants you access to remote clinicians anywhere, not just locally.
/Prime-Care-Technologies-Logo.png?width=191&height=55&name=Prime-Care-Technologies-Logo.png)

/PCT-Trans.png)

